Flu vaccines do more than protect one person. They help keep whole communities safe. These shots build community immunity and stop big outbreaks. At DrMorepenHome.com, we know vaccines protect both individuals and entire neighborhoods.
How Flu Vaccines Create Community Immunity
Community immunity works like a shield. When many people get vaccinated, fewer germs spread around. This protects people who can't get vaccines themselves.
How Vaccines Protect Everyone
Flu vaccines teach your body to fight the flu virus. Your immune system learns to recognize the virus. If the real virus shows up later, your body knows what to do.
Here's what happens:
- Your body makes antibodies to fight flu germs
- You're less likely to get sick
- You won't spread the virus to others as easily
- People around you stay safer
When lots of people get vaccinated, the whole community benefits. Even babies and people with weak immune systems get protection.
What Is Herd Immunity?
Herd immunity happens when enough people are protected from a disease. The disease can't spread easily anymore. It's like building a wall around your community.
How many people need vaccines?
The number depends on how easily the disease spreads. For flu, we need many people vaccinated to build strong protection.
Who gets protected?
Everyone benefits, especially people who can't get vaccines. This includes very young babies and people with certain health problems.
The goal is simple: make flu outbreaks rare and less severe.
%20(1).png)
Real Examples of Community Protection
We can see how well vaccines work by looking at real situations:
Japan's school program: In the 1960s and 1970s, Japan gave flu shots to school children. Fewer elderly people died from flu. Kids getting vaccines protected their grandparents too.
Yearly vaccine programs: Cities with good vaccine programs see less flu every year. The vaccines work best in crowded places where germs spread fast.
COVID-19 lessons: The pandemic showed us how important vaccines are for community health. The same rules that worked for COVID work for flu too.
These examples prove that vaccines help everyone, not just the person getting the shot.
Why Public Health Needs Flu Vaccination
Flu spreads fast and makes many people very sick. Good vaccination programs stop this from happening.
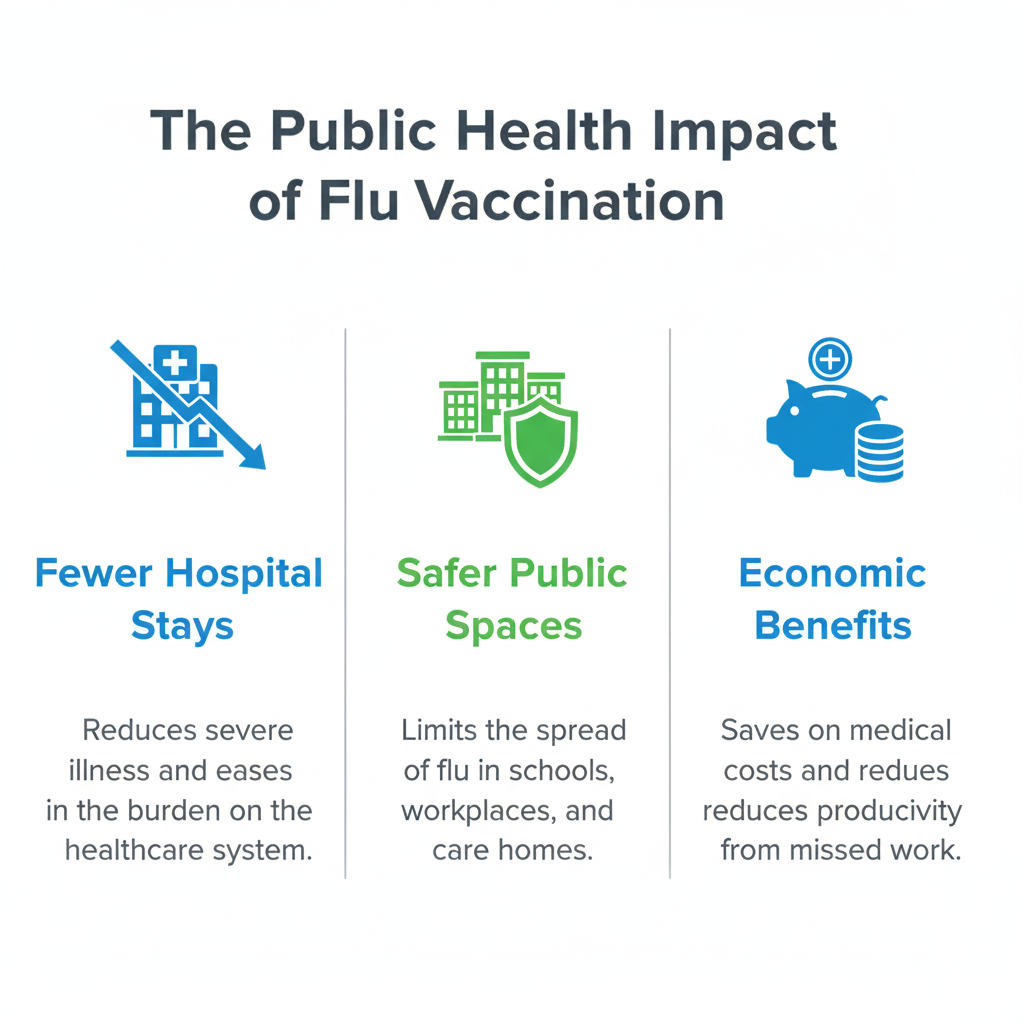
Stopping Flu in Public Places
Schools and workplaces: These places have lots of people close together. Vaccines stop flu from spreading in classrooms and offices.
Nursing homes and hospitals: Older adults and sick people need extra protection. High vaccination rates keep these places safer.
Teaching people about vaccines: When people understand how community immunity works, more get vaccinated.

Fewer Hospital Visits and Deaths
Vaccines save lives in several ways:
- Fewer people need hospital care
- Flu complications happen less often
- Fewer people die from flu-related illness
These improvements show why vaccines matter so much for public health.
Money Benefits of Vaccination
Vaccines save money too:
- Lower medical bills for everyone
- People miss less work when they don't get sick
- Hospitals don't get overwhelmed
- The whole healthcare system works better
Good vaccination programs pay for themselves many times over.
How Flu Vaccines Stop Outbreaks
Vaccines are our best defense against big flu outbreaks.
When Vaccines Prevented Disasters
2009 Swine Flu: Quick vaccine programs helped control H1N1 flu spread worldwide.
Comparing different areas: Places with more vaccinated people always do better during flu season.
Understanding Breakthrough Cases
Sometimes vaccinated people still get flu, but vaccines still help:
- Symptoms are usually much milder
- People recover faster
- They're less likely to spread flu to others
Scientists keep working to make vaccines even better.
.png)
What the Numbers Tell Us
Vaccine success varies each year. The match between vaccine and circulating flu strains matters. But getting vaccinated year after year builds strong community protection.
Building Better Vaccination Programs
Strong vaccination programs need several things to work well.
Making Vaccines Easy to Get
Multiple locations: Vaccines should be available at pharmacies, schools, and community centers. Dr. Morepen Home works with local partners to increase access.
Affordable cost: Insurance should cover vaccines. Free programs help people who can't afford them.
Convenient times: Weekend and evening hours help working people get vaccinated.
Reward programs: Small incentives can encourage more people to get their shots.

Teaching Communities About Vaccines
People need good information to make smart choices about vaccines.
Public campaigns: Social media and news stories can share vaccine success stories.
Community workshops: Local health experts can answer questions and address concerns.
Partnership efforts: Schools, businesses, and community groups can work together. Dr. Morepen Home provides educational materials and expert advice for these efforts.
Healthcare Workers as Leaders
Doctors and nurses have people's trust. They play a key role in promoting vaccines.
Direct conversations: Healthcare workers should talk about vaccines during regular visits.
Staying updated: Medical staff need current information about vaccine benefits and safety.
Community influence: Respected local leaders can help spread the vaccine message.
Dr. Morepen Home trains healthcare professionals to discuss flu vaccination confidently and clearly.
Addressing Vaccine Concerns
Many people worry about vaccine safety. Honest answers help build trust.
Safety and Side Effects
Vaccines go through strict testing before approval.
Common side effects: Sore arm or mild fever that goes away quickly.
Serious reactions: These are extremely rare. Vaccination sites can handle them if they occur.
Safety monitoring: Government systems track vaccine safety constantly.
Being honest about both benefits and risks helps people make good decisions.
Common Vaccine Myths
Myth: "I never get flu, so I don't need the vaccine."
Truth: Past health doesn't predict future illness. Flu strains change every year.
Myth: "Flu is just a bad cold."
Truth: Flu can cause serious illness, hospitalization, and death.
Myth: "The vaccine can give you flu."
Truth: Vaccine viruses are weakened or killed. They can't cause flu illness.
Dr. Morepen Home helps communities understand these facts.
Questions People Ask Most
Does the vaccine work? Effectiveness ranges from 40% to 60%, but it still reduces illness severity significantly.
When should I get vaccinated? Early fall is best, usually October or November.
Do children need special doses? Some young children need two doses their first time.
Clear answers from trusted sources like Dr. Morepen Home reduce vaccine hesitancy.
The Future of Flu Vaccination
New technology will make vaccines better and easier to use.
New Vaccine Development
Universal flu vaccines: Scientists want to create vaccines that work against many flu types. This could eliminate yearly shots.
Better delivery methods: Patches or nasal sprays might replace needles someday.
These advances could make vaccination easier and more effective.
Global Vaccine Efforts
Flu viruses cross borders easily. International cooperation helps everyone.
World partnerships: Organizations like WHO and CDC work to improve vaccine access worldwide.
Fair distribution: All communities need access to vaccines for global protection to work.
Dr. Morepen Home supports global health goals in local practice.
Learning from COVID-19
The pandemic taught important lessons:
Distribution systems: Efficient vaccine delivery is crucial for success.
Public trust: Clear communication and transparency build confidence in vaccines.
Community strength: Strong health systems help communities handle health challenges better.
Dr. Morepen Home uses these lessons to improve flu vaccination efforts.
Conclusion
Flu vaccines protect individuals and strengthen entire communities. They create community immunity that shields vulnerable people who can't get vaccinated themselves. This includes babies and people with health conditions who need extra protection.
DrMorepenHome.com believes building healthier communities is everyone's job. When you get vaccinated, you help protect your neighbors, coworkers, and family members. Your personal choice has community-wide benefits.
We must keep teaching people about vaccine benefits. We need to support efforts that make vaccines available to everyone. Each person who gets vaccinated adds to our community's protection.
Together, we can face each flu season with confidence. Every vaccine given builds stronger immunity for all of us.
Frequently Asked Questions
Why should healthy people get flu vaccines?
Healthy people can still carry and spread flu to others. Your vaccination protects vulnerable people around you and helps build community immunity.
Can flu vaccines give you the flu?
No. Flu vaccines use killed viruses or virus pieces that can't cause illness. Some people feel mild achiness afterward, but this isn't the flu.
Why do flu vaccines change each year?
Flu viruses change constantly. Scientists update vaccines each year to match the strains expected that season.
Are there serious side effects?
Serious reactions are extremely rare. Most people only experience mild soreness where they got the shot or a slight fever.
When is the best time to get vaccinated?
Early fall is ideal, but getting vaccinated later still provides protection. Flu season often peaks in winter and can last into spring.
At DrMorepenHome.com, we're committed to supporting your health with reliable information and caring service.
.png)



.png)
.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)
.png)

.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)

.png)
.png)
.png)

.png)

.png)


.png)







