Dealing with chronic illness is a constant journey. Patients with conditions like diabetes, heart disease, hypertension, or arthritis face persistent obstacles that demand more than just medicine. Chronic illness management involves regular monitoring, adapting daily habits, and finding the right treatment plan for long-term stability. Nursing support stands at the heart of this process, providing steady guidance not just in clinics or hospitals, but often right at home.
Understanding Chronic Illness: What It Means and What It Changes
A chronic illness is a medical condition that lasts for a long period—often years—and requires ongoing management rather than a cure. These conditions impact daily living, emotional health, and family routines. Many patients shoulder the weight of complicated medication schedules, dietary restrictions, frequent doctor appointments, and lifestyle adjustments. Facing these hurdles alone can feel overwhelming.
What sets chronic care apart is the need for continuous support. Nurses step in as trusted partners, helping patients understand their health, stay on track with treatments, and adjust their lifestyle to match medical recommendations. Their involvement brings order and reassurance to daily life, often making health goals more achievable.
%20(1).png)
Nurses: The Core of Chronic Illness Management
Nurses have always played a crucial part in healthcare. Yet, in chronic illness management, their role expands far beyond basic patient care. They cover patient assessments, implement care plans, provide education, offer emotional support, and coordinate with other healthcare professionals. Nursing support creates a bridge between complex medical systems and the real-world needs of each patient.
Patient Assessment and Monitoring
Nurses consistently monitor vital signs, symptoms, and mental well-being. Regular assessments form the basis for adapting care when patients face changes—whether it’s a new symptom or a shift in how they respond to treatment. This vigilance helps catch problems early, making timely intervention possible.
Creating and Adjusting Care Plans
Each patient’s history and experience with their illness is different. Nurses develop customized care plans, factoring in medical history, lifestyle, and emotional state. Since chronic conditions often change over time, nurses remain alert, making adjustments as needed. This flexible, personalized approach ensures patients always have support tailored to their unique situation.
Coordinating With Healthcare Teams
For comprehensive care, nurses make sure communication flows smoothly between doctors, therapists, nutritionists, and others. They keep everyone updated on changes in the patient’s status or treatment. This teamwork protects against confusion and ensures no step is missed in the journey toward better outcomes.
Why Nursing Support Makes a Difference
Nursing support stands out for its holistic approach—looking after the whole person, not just the disease. By forging strong relationships, nurses encourage patients to follow treatment plans, manage stress, and get the most from available resources. This active involvement improves clinical outcomes and helps patients develop lasting skills to manage illness independently.

Benefits of Nurse-Led Care
- Improved Outcomes: Regular monitoring, timely changes to treatment, and ongoing education lead to fewer hospitalizations and better-managed symptoms.
- Better Quality of Life: With reliable nursing support, patients handle pain, fatigue, and lifestyle changes more successfully. Nurses provide strategies for coping, making daily activities less daunting.
- Empowered Self-Care: Nurses teach patients and families about their condition, treatment options, and how to track progress. This practical knowledge increases confidence and encourages patients to take charge of their health.
Key Nursing Responsibilities in Action
Assessment and Monitoring Techniques
Nurses use check-ups, questionnaires, and technology to measure vital signs, watch for new symptoms, and gauge mental health. Wearable devices and telehealth have made it easier to stay connected, even from home.
Implementing and Revising Care Plans
Plans are never static. Nurses adapt strategies as they see changes—maybe increasing check-ins for a patient with fluctuating blood sugar or providing extra help if someone is struggling with new medications.
Coordinating Care
Nurses act as a hub, connecting patients with medical specialists, mental health support, dietitians, or physiotherapists. Regular team meetings, shared records, and clear patient feedback make sure everyone works together.
Nurse-Led Strategies for Success
Prevention
By teaching patients about warning signs and the importance of regular screenings, nurses help prevent worsening of chronic conditions.
Lifestyle Modification
Patients often need to make big changes—diet, exercise, quitting smoking, or stress management. Nurses show doable steps, check in on progress, and celebrate successes to keep motivation strong.

Medication Management
Nurses teach patients about medication schedules, what side effects to watch for, and how to handle missed doses, helping reduce medication errors and complications.
Education
Clear, jargon-free language is key. Nurses explain test results, what the numbers mean, and why certain steps matter. Educational handouts, videos, and even small group workshops are often used to keep learning interactive.
Real Results and Patient Stories
Research shows that nurse-led programs cut hospital admissions and boost satisfaction. Take, for example, a patient with diabetes who, working with a nurse, starts recording daily glucose readings, attends regular nutrition sessions, and discusses progress by phone. Over time, blood sugar stabilizes and emergency hospital visits drop.
A heart patient might receive weekly home visits where a nurse tracks blood pressure, checks in on medication adherence, and motivates gradual exercise. When problems arise, immediate action is possible. These stories show the impact of sustained, personalized nursing support.
.png)
Barriers and Future Directions
There are real challenges:
- Resource Constraints: Many healthcare settings have limited staff and growing caseloads.
- Patient Compliance: Not everyone finds it easy to stick to new habits, even with support.
- Changing Healthcare Landscape: New conditions and treatments keep appearing, requiring nurses to learn and adapt continuously.
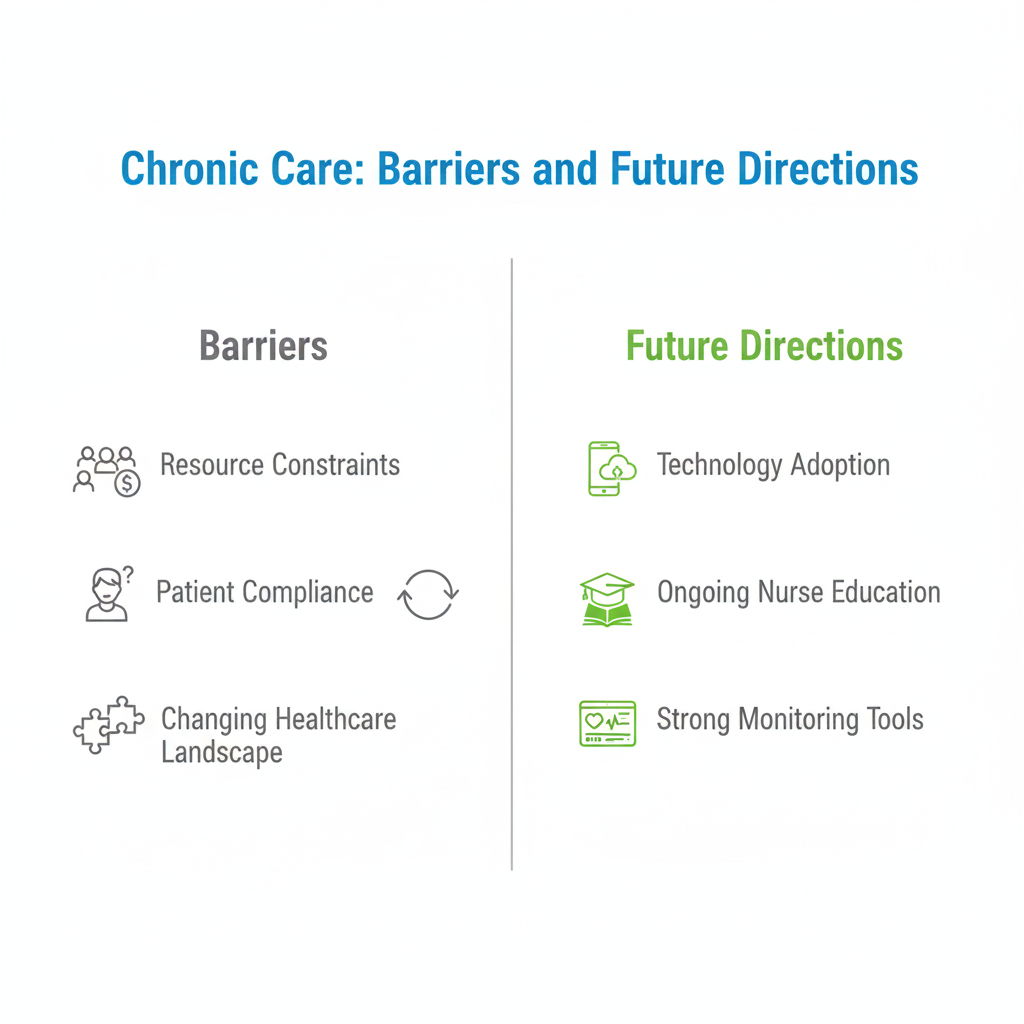
Despite the hurdles, the future for nurse-led chronic illness management is promising. Technology, like smart devices and telemedicine, is helping nurses stay ahead. Organizations such as Dr. Morepen’s Home Health Services invest in ongoing nurse education and strong tools for patient monitoring, ensuring nurses remain equipped for these evolving demands.
Conclusion
Chronic illness is a lifelong challenge, but with nursing support at the center, patients find strength, stability, and hope. Nurses bring structure to complicated care routines and become allies in every patient’s day-to-day health journey.
With their blend of medical expertise, personal care, and problem-solving, nurses are essential in shaping improved outcomes and a better life for those living with chronic conditions. Organizations focused on supporting and empowering nurses—like Dr. Morepen’s Home Health Services—will continue to drive innovation and compassion in chronic illness management for years to come.
.png)



.png)
.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)
.png)

.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)

.png)
.png)
.png)

.png)

.png)


.png)







