Digestive discomfort is common when daily pressures rise. Many people notice changes in their gut without realizing stress could be a driving force. Understanding how stress impacts digestion is essential for finding relief and long-term balance. At Dr. Morepen Home, we care about everyday health and real-world solutions. In this guide, discover how stress affects the gut, which symptoms to look for, and actionable ways to support digestive strength.
How Stress Alters Digestive Function
The Brain-Gut Connection: Signaling and Responses
The gut and brain are closely linked through a network of nerves and chemical signals. When worries build up, these signals change, sometimes making digestion unpredictable. Some call the gut the "second brain" because it responds so quickly to emotional triggers. Stomach pain before an event or changed bowel habits during tough times are often signs of this connection in action.
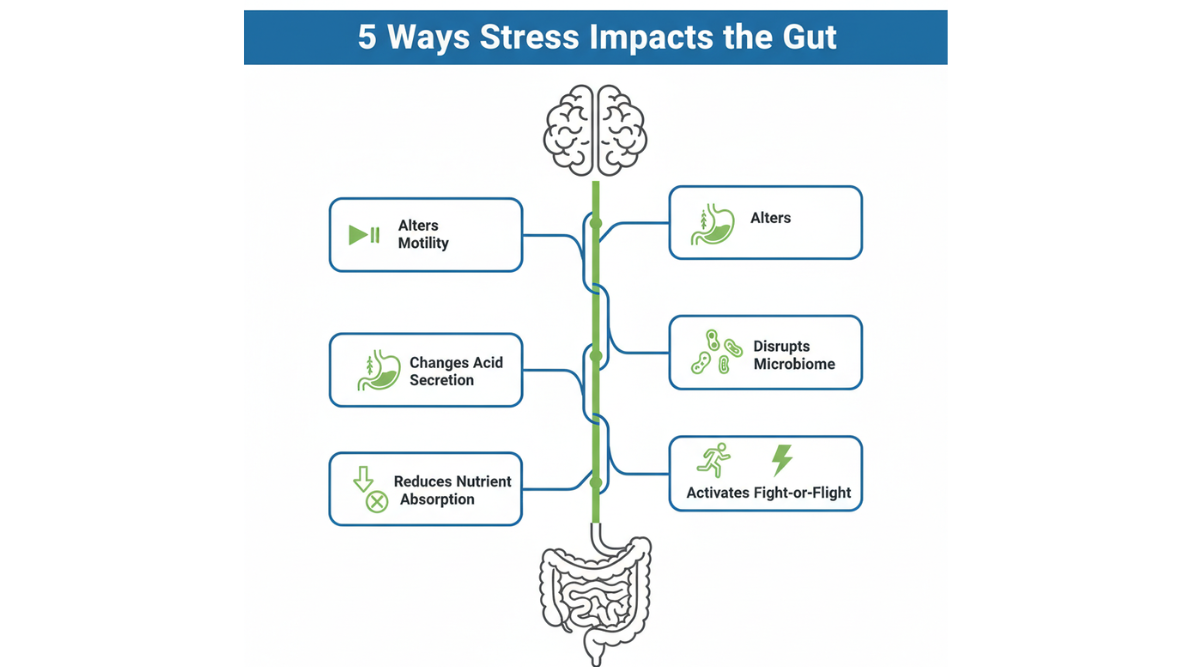
Fight-or-Flight Effects on Gut Motility
Stress activates the body’s fight-or-flight system. During this response, digestion often pauses. Blood flows away from the stomach and intestines to the muscles and heart. You might notice food moves more slowly or much faster, causing constipation or diarrhea.
Changes in Stomach Acid and Secretion Patterns
Emotional strain can increase or decrease stomach acid. This sometimes leads to indigestion, heartburn, or reflux. If stress is ongoing, these problems can feel worse or happen more often.
Microbiome Disruption and Bacterial Imbalance
Periods of stress may disturb the balance of gut bacteria. This can lead to bloating, gassiness, or extra sensitivity in the digestive tract. The gut microbiome helps regulate nutrient breakdown immunity, and even mood.
Nutrition Absorption & Metabolic Shifts
When under pressure for days or weeks, the digestive system can absorb nutrients less efficiently. This may drain energy, cause subtle deficiencies, and lead to lingering tiredness.
Common Digestive Issues Triggered by Stress
Indigestion and Heartburn
Upset stomach, burning in the chest, or a heavy sensation after meals may all flare up when life feels too heavy. These problems sometimes emerge alongside stressful events or emotional conflicts.
Bloating, Gas, and Stomach Pain
A bloated belly, more gas than usual, or sudden aches are common when your body’s stress response affects the gut. This can happen repeatedly during the day or seem to show up without an obvious reason.
Diarrhea, Constipation, and Irregularity
Stress can slow or speed up how food moves through the digestive system. Some people rush to the bathroom often, while others become more constipated. The pattern can change every few days, driven by mood and mental strain.
Appetite Changes: Overeating vs Loss of Appetite
When stress lingers, some people eat more, seeking comfort in food. Others skip meals or have no desire to eat. These shifts add confusion to daily routines and can create ongoing gut trouble.
Nausea, Cramps, and General Discomfort
Not all stomach distress is physical. Nausea, random cramps, or a dull, nervous feeling in the gut may appear during high-pressure periods, then resolve as things calm down.
Long-Term Risks: When Stress Leads to Persistent Problems
Stress and Chronic Disorders (IBS, IBD, GERD)
Living with chronic gut trouble, like irritable bowel syndrome, inflammatory bowel disease, or acid reflux? Ongoing stress can worsen flare-ups for these conditions, even though it does not create them.
Recurring Digestive Symptoms: Warning Signs
If stomach pain, erratic bowel habits, or heartburn happen often, it may be time to look deeper. Persistent stress can turn brief symptoms into frequent episodes, making quality of life suffer.
Impact on Immune Function and Inflammation
Long-lasting worry affects how the body fights infection in the gut. Heightened inflammation may follow and can raise the odds of getting food poisoning or sensitivities to common foods.
When to Consult a Doctor for Digestive Complaints
Reach out to a healthcare provider if digestive symptoms stick around for weeks, get much worse, or are joined by weight loss, bleeding, or severe discomfort. Early attention can prevent bigger problems down the line.
Causes and Triggers: Why Stress Affects Your Gut
Emotional and Mental Health Stressors
Daily anxiety, feeling low, or never-ending worries all take a toll on the gut. These emotional triggers may be obvious or subtle, but the gut often reacts first.
Physical Stress (Illness, Exhaustion, Pain)
Physical ailments, a bout of the flu, or plain exhaustion hit the digestive system hard. Pain or increased demands on the body are common drivers for gut changes.
Lifestyle Factors (Sleep Loss, Poor Nutrition)
Skipping sleep or grabbing fast food between calls? These habits worsen how the gut reacts to stress and may draw out symptoms.
Environmental and Occupational Stress
Work deadlines, busy home lives, and noisy surroundings can affect the gut by increasing tension even when you think you’ve adjusted.
Gut-Brain Feedback Loops - the Vicious Cycle
Gut symptoms can boost anxiety, and in turn, anxiety makes gut symptoms worse. Breaking this cycle through both mental and physical strategies leads to better digestive health over time.
Recognizing the Symptoms: What to Watch For
Digestive Warning Signs Linked to Stress
Notice any of these gut problems during tough times?
- Frequent stomach aches, cramps, or bloating
- Burning or discomfort after meals
- Sudden changes in bowel habits - diarrhea or constipation
- A feeling of fullness or gassiness that comes and goes
Track these changes in a notebook or on your phone. Patterns often appear as stress ebbs and flows.
Emotional Symptoms Accompanying Gut Issues
Gut problems and mental strain go hand in hand. Watch for:
- Anxiety, restlessness, or irritability
- Loss of focus or trouble sleeping
- Feeling “on edge” or tight in the chest during stomach pain
These emotional flags often lead existing digestive symptoms to worsen.
Red Flags for Serious Conditions
Some symptoms indicate you should contact a doctor soon:
- Severe pain lasting over a week
- Unintended weight loss
- Blood in stool or vomit
- Ongoing nausea with no clear cause
Don’t ignore these signs - quick care makes a big difference.
Effective Strategies for Managing Stress-Induced Digestive Symptoms
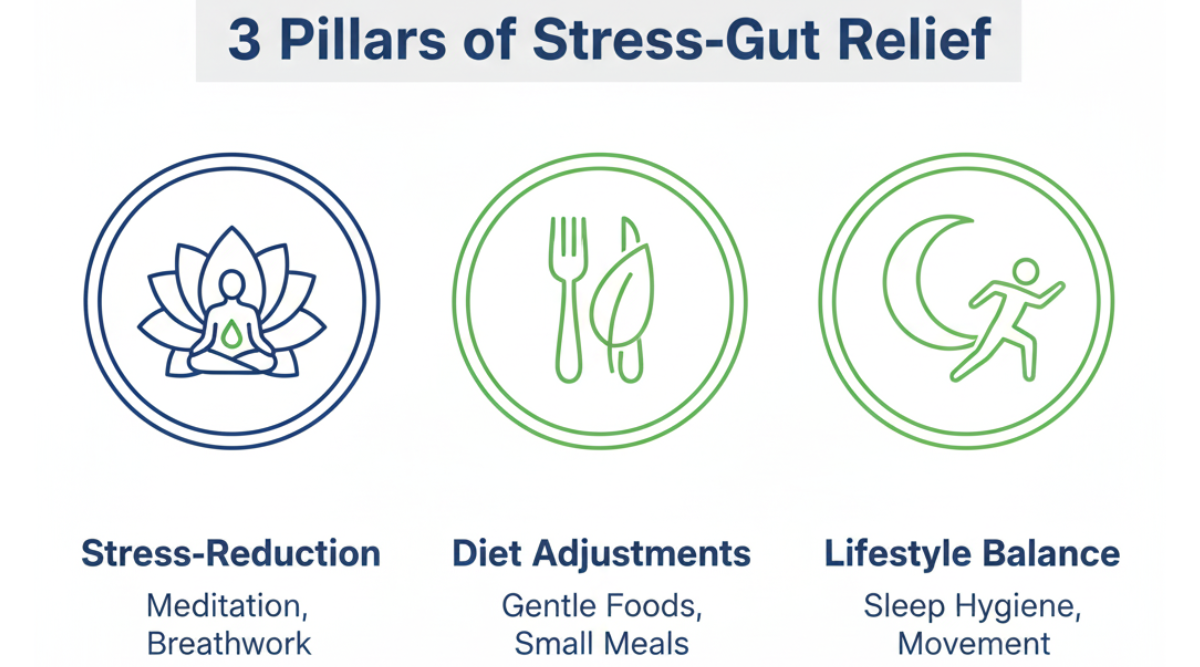
Stress-Reduction Techniques (Breathwork, Meditation, Mindfulness)
Simple steps help:
- Slow, deep breathing for five minutes
- Guided meditation apps for calming the mind
- Taking quiet breaks from screens or busy spaces
These tools lower the body's stress levels, giving your gut time to steady itself.
Diet Adjustments for Sensitive Stomachs
Try choosing foods that comfort the gut:
- Oats, bananas, curd, rice - easy on digestion
- Cooked vegetables instead of raw salads
- Smaller, more frequent meals rather than large portions
Keep spicy, fatty, or very sweet foods to a minimum until symptoms improve.
Physical Activity and Movement Benefits
Regular activity helps:
- Gentle walks, yoga, or stretching
- Movement boosts digestion and eases tension
Don’t overdo high-impact sports or workouts during bad flare-ups.
Sleep Hygiene for Digestive Health
Aim for consistent rest:
- Go to bed and wake up at regular times
- Avoid screens before sleep
- Create a calm, cool bedroom
Sleep restores balance to both gut and mind.
Home Remedies and OTC Relief Options
Home fixes to consider:
- Ginger tea for mild nausea or pain
- Warm compresses for cramping
- Over-the-counter antacids or probiotics (talk to a doctor first)
These can help but shouldn’t replace medical advice for serious problems.
Building Resilience: Long-Term Prevention Tactics
Creating Daily Stress Management Habits
Develop routines such as:
- Morning deep breathing
- Evening gratitude lists
- Taking short breaks throughout your workday
Little habits lower stress and build long-term resistance.
Strengthening Gut Health with Probiotics and Prebiotics
Add foods like curd, buttermilk, and fermented vegetables to meals. These support balanced gut bacteria and promote healthy digestion.
Meal Timing and Mindful Eating Approaches
Eat around the same time each day. Put away devices during meals. Chew slowly to give your body time to signal fullness.
Balancing Work, Life & Mental Health for Gut Wellness
Check for signs of burnout, adjust work loads when possible, and seek help when stress feels overwhelming. Social support is a powerful buffer for gut health.
When to Seek Medical Help
Chronic or Worsening Symptoms
If gut trouble keeps getting worse or won’t go away, talk to a doctor. Addressing these issues early ensures better results.
How Doctors Diagnose Stress-Linked Digestive Issues
A doctor may:
- Ask about your symptom patterns and stress levels
- Suggest tests - bloodwork, stool tests, or imaging
- Discuss referral to a dietitian, counselor, or gut health specialist
Expected Tests and Specialist Referrals
Tests might check for infections, inflammatory markers, or digestive function. Specialists tailor solutions to your health needs.
FAQs
Can stress really cause severe gut problems?
Yes. Stress influences the entire digestive tract, making symptoms mild or severe depending on your situation.
What are quick fixes for stress-related stomach pain?
Try deep breathing, sipping ginger tea, gentle walking, or resting in a dark room. For lasting help, address both stress and gut triggers.
Are digestive issues always caused by stress or could it be something else?
Stress is one major factor, but infections, food intolerances, and medical conditions may also play a role.
How can I tell if my gut symptoms are stress-related?
Symptoms appear or get worse during tension. Relief typically follows as stress lowers.
Will relaxation techniques help with digestive disorders?
Most people report some improvement when they regularly practice stress relief.
.png)


.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)


.png)
.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)
.png)

.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)

.png)
.png)
.png)

.png)

.png)


.png)







