Flu vaccines help protect people from getting sick each year. Learning about how well these vaccines work is important for doctors and regular people too. In 2023, new flu strains keep appearing, so we need to understand how vaccines fight them. This blog will look at recent studies and explain what makes flu vaccines work better or worse.
Current Understanding of Flu Vaccine Effectiveness
What Recent Studies Show About Flu Vaccines
Scientists study flu vaccines every year to see how well they work. Many things make this tricky to measure. The vaccine ingredients and a person's health both matter a lot.
The CDC has done big studies. They found that flu vaccines lower the chance of getting flu by 40% to 60%. This happens when the vaccine matches the flu strains going around.
No vaccine works 100% of the time. But flu vaccines do help reduce how sick people get. They also keep people out of hospitals. For example, recent data shows fewer people went to hospitals for flu after getting vaccinated.
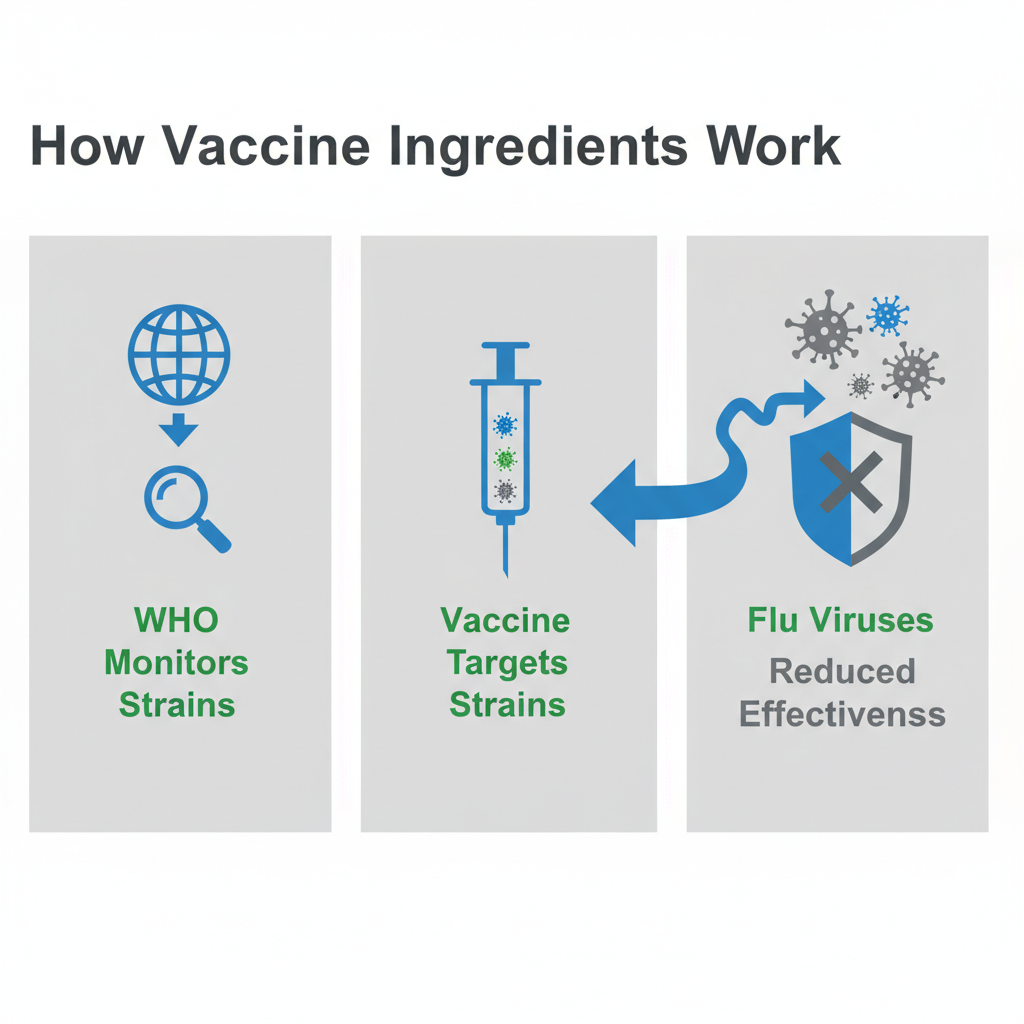
How Vaccine Ingredients Affect How Well They Work
What goes into a flu vaccine really matters. Each year, the World Health Organization looks at flu virus strains. They pick which ones should go in vaccines.
The goal is to match the vaccine to the flu strains that will spread. But flu viruses change often. When they change too much, the vaccine might not work as well. This makes flu vaccines harder to predict than other vaccines.
Some vaccines target three flu strains. Others target four strains. Having more strains in one shot can help protect against more types of flu.
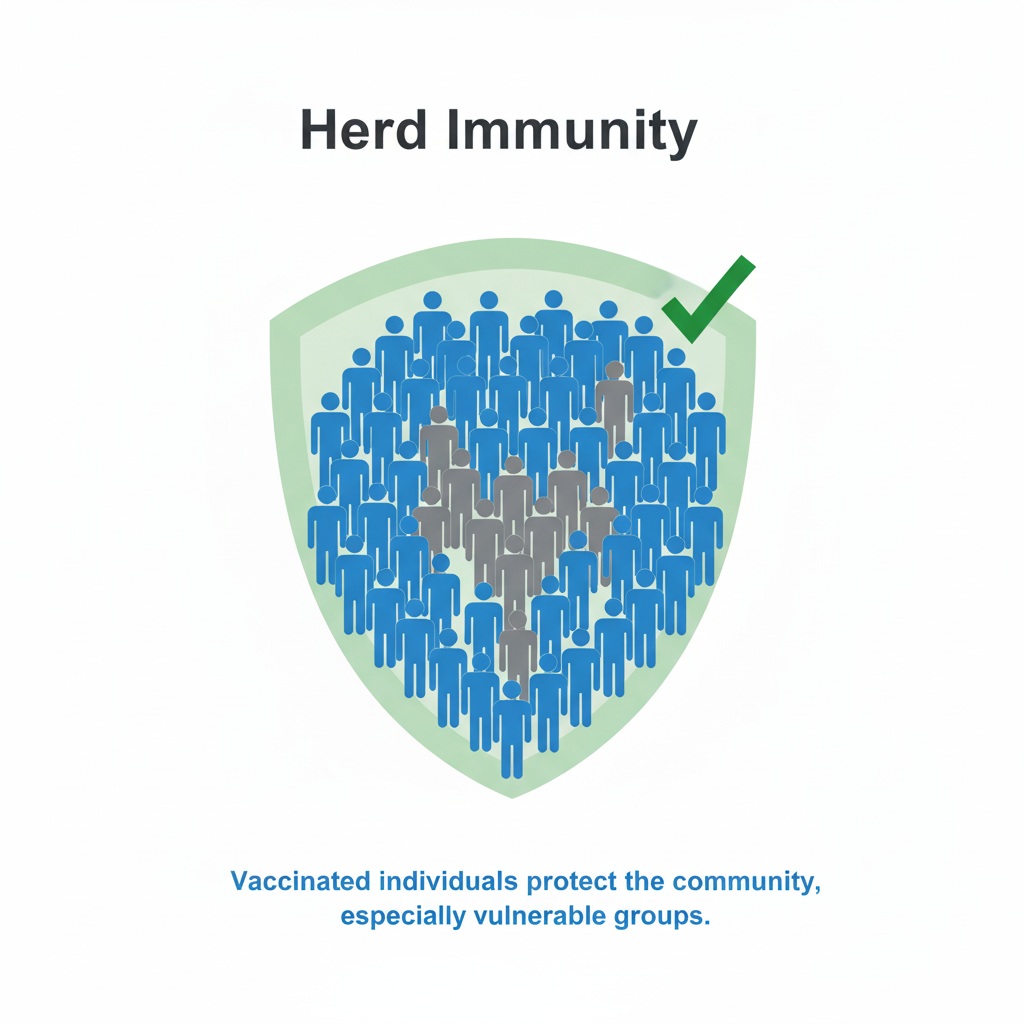
How Community Protection Helps Stop Flu
When lots of people in a community get vaccinated, it helps protect everyone. This is called herd immunity. It works especially well for people who can't get vaccines because of health problems.
Kids, elderly people, and those with chronic diseases benefit the most. The more people who get vaccinated, the less flu spreads around. This creates a shield of protection for the whole community.
Public health campaigns and good policies help more people get vaccinated. When vaccination rates go up, everyone stays healthier.
Looking at Flu Vaccine Success Over Time
How Protection Rates Change Each Year
Flu shot protection has gone up and down over the years. The main reason is whether the vaccine matches the flu strains going around. Historical data shows effectiveness between 40% and 60% most years.
This variation makes it hard for health organizations. They have to keep improving how they make and give out vaccines.
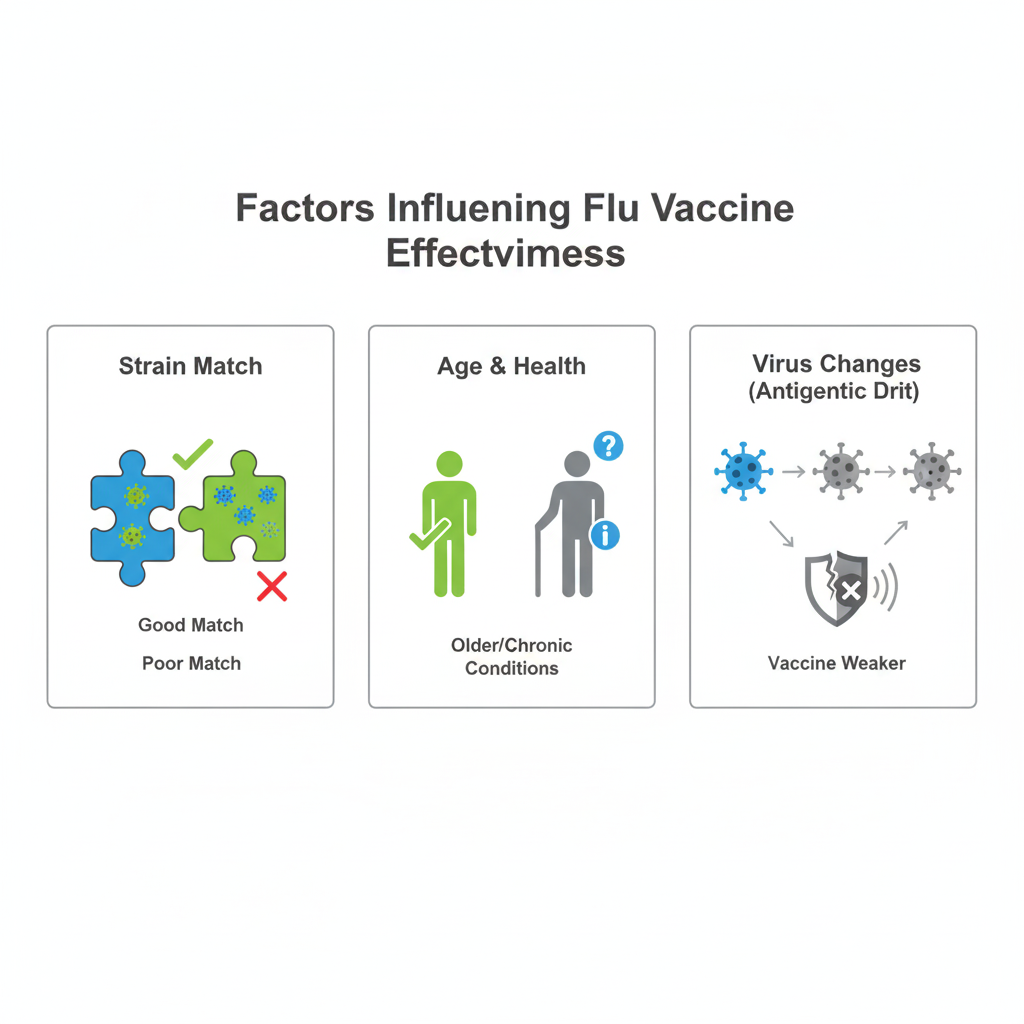
How Different Groups Respond to Flu Vaccines
Not everyone responds to flu vaccines the same way. Healthy adults usually get good protection. Older adults and people with chronic diseases might not get as much protection.
This happens because immune systems work differently as people age. Some health conditions also make immune systems weaker.
Special high-dose vaccines work better for older people. Kids tend to respond really well to flu vaccines. This helps keep children out of hospitals during flu season.
How Virus Changes Affect Vaccine Success
Flu viruses change their genetic makeup all the time. Scientists call this antigenic drift. When viruses change a lot, vaccines might not work as well.
In years when big changes happen, vaccine effectiveness can drop. But scientists have gotten better at adapting vaccines quickly. This helps minimize the impact when viruses change.
Scientific Evidence from Recent Flu Seasons
Real-World Examples of Vaccine Impact
Recent case studies show flu vaccines help even when they don't work perfectly. During the 2019-2020 flu season, vaccines prevented thousands of flu cases. They also kept many people out of hospitals and saved lives.
These studies use real-world data. They show vaccines help reduce serious outcomes even in tough years.
%20(1).png)
Data from Health Agencies
The CDC and other health agencies collect lots of data about vaccines. This information helps researchers understand how vaccines work on a large scale. Advanced computer programs help analyze this data.
The data shows vaccines don't just prevent flu. They also reduce the burden on hospitals and healthcare systems.
How Public Campaigns Help
Public vaccination campaigns make a big difference. They teach people about vaccine benefits and clear up myths. More people get vaccinated when campaigns work well.
Recent campaigns use social media and websites to reach more people. This helps spread accurate information about vaccines to larger audiences.
Good public health strategies need many different approaches. They combine education, easy access to vaccines, and supportive policies.
What Affects How Well Flu Vaccines Work
Age, Health, and Vaccine Response
People respond differently to flu vaccines. Age plays a big role. Older adults might not get as much protection because their immune systems work differently as they age.
Young healthy adults and children usually respond better. Their immune systems are stronger and can fight off flu better after vaccination.
People with chronic diseases like heart problems, asthma, or diabetes might need special vaccines. Their health conditions can change how well vaccines work. Doctors might recommend high-dose vaccines for these patients.
Why Matching Vaccine Strains Matters
How well vaccine strains match circulating viruses is really important. Each year, scientists try to predict which flu strains will cause the most illness. They use this information to make vaccines.
When scientists guess right, vaccines work much better. When they guess wrong, effectiveness goes down. This shows why global monitoring of flu patterns is so important.
Organizations like the WHO watch flu patterns all over the world. They update vaccine recommendations to give people the best protection possible.
Outside Factors That Affect Vaccines
Many outside factors can change how well flu vaccines work. Where you live, when you get vaccinated, and even the weather can make a difference.
Flu activity varies by region and year. Public health policies in different places also affect how vaccines work.
Timing matters too. Getting vaccinated too early or too late can reduce protection. The best time is before flu season gets busy. This gives your body time to build immunity.
Weather conditions like humidity and temperature affect how flu spreads. This indirectly impacts how effective vaccines are.
Benefits and Side Effects of Flu Vaccines
Common Side Effects and How to Handle Them
Flu vaccines can cause mild side effects. Most people only have minor problems that go away quickly. Common side effects include sore arm, low fever, headaches, and muscle aches.
These symptoms usually last only a few days. Over-the-counter pain medicine and rest can help. Understanding these minor risks helps people make good decisions about vaccination.
Teaching people about side effects honestly can reduce fear about vaccines. This helps more people choose to get vaccinated.
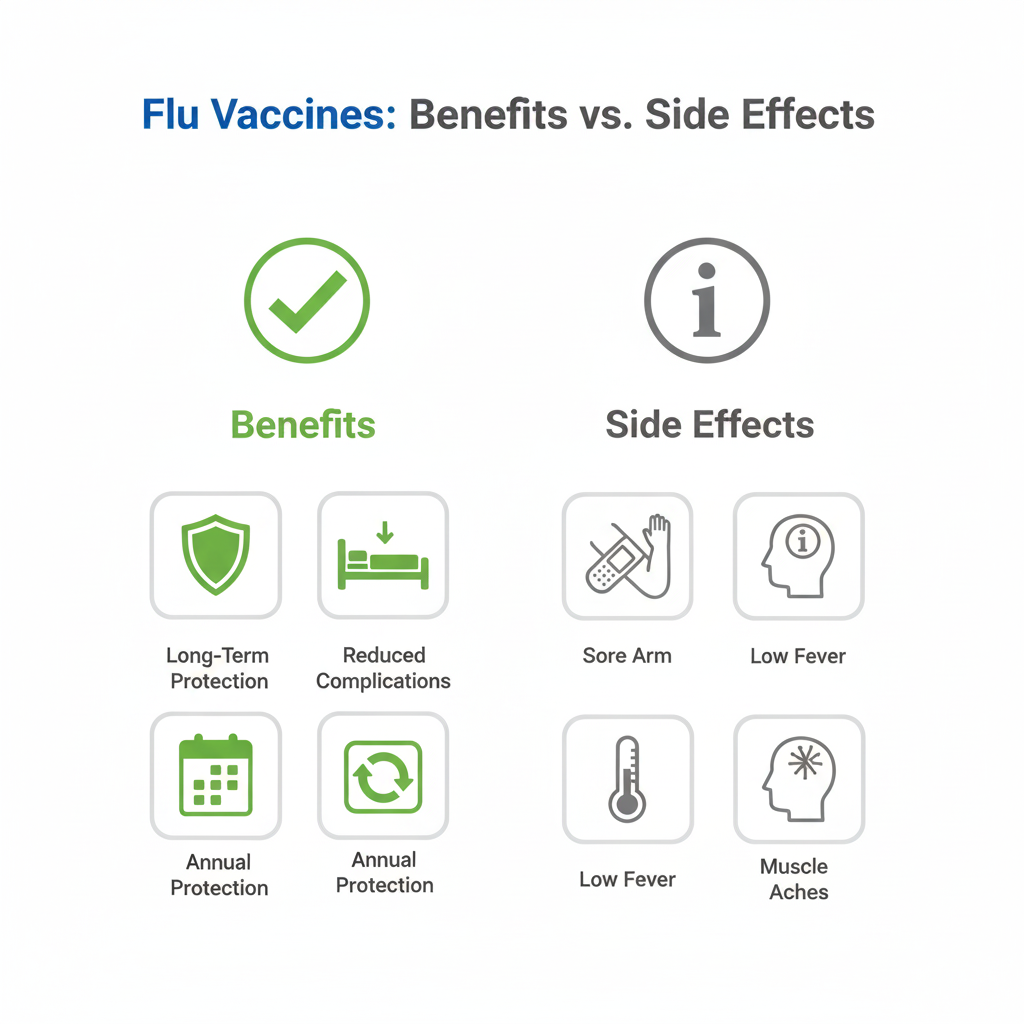
Long-Term Benefits of Getting Vaccinated Every Year
Getting flu shots every year provides protection that builds over time. Regular vaccination might help create stronger immunity that lasts longer.
Preventing flu consistently also reduces complications. This includes problems like pneumonia or worsening of chronic conditions. These benefits can help people stay healthier for years.
Safety Records of Different Flu Vaccines
Flu vaccines have excellent safety records. Extensive research shows they are safe for most people. Different types of vaccines work for different groups.
High-dose vaccines work well and safely for older adults. Live vaccines are good for younger, healthy people. Scientists continue to monitor vaccine safety to make sure benefits outweigh risks.
Public Health Impact of Flu Vaccine Effectiveness
Vaccination Rates and Community Health
How many people get flu vaccines affects the whole community's health. Higher vaccination rates mean fewer flu cases and less spreading. This also reduces strain on hospitals and clinics.
Public health agencies work to improve vaccination rates. They address barriers like cost and access. They also educate people about vaccine benefits.
Getting vaccines to enough people in a community protects everyone. This is especially important during bad flu seasons.
.png)
Policy Ideas for Flu Season
Good flu vaccination policies balance public health goals with making vaccines accessible and affordable. Strategies include workplace vaccination programs and integrating vaccines into regular medical care.
Policies also focus on reaching high-risk groups. Making sure these people get timely vaccinations helps prevent serious outcomes.
Low-cost or free vaccines encourage more people to get vaccinated. This helps achieve better community protection.
Future Vaccine Development
Research into flu vaccines keeps improving. Scientists want to make vaccines that work better and last longer. New technologies like mRNA vaccines show promise.
Universal flu vaccines that target parts of the virus that don't change much could provide longer-lasting protection. This would be a major breakthrough.
AI tools can help predict flu outbreaks and identify vaccine strains faster. Technology will play a big role in improving flu vaccines in the future.
Conclusion
Understanding how flu vaccines work helps us make better health decisions. Flu vaccines serve as protection for individuals and communities. Even though effectiveness varies year to year, vaccines remain crucial for reducing flu's impact.
Each year's vaccine composition depends on predicted strains and ongoing virus changes. This shows how dynamic vaccine development really is. Herd immunity becomes more important as we adapt to these changes.
Data and case studies confirm that flu vaccines reduce serious outcomes and healthcare burdens. This emphasizes the need for strong vaccination campaigns that reach many people. Health organizations, healthcare workers, and individuals must work together.
Continued research and innovation will be key to improving vaccines. This will lead to better formulations and strategies that work for more people.
Staying informed and committed to flu vaccination protects personal health and strengthens community resilience. With good choices and proactive health measures, we can handle flu seasons with confidence and work toward a healthier future.
Frequently Asked Questions
How is flu vaccine effectiveness measured?
Flu vaccine effectiveness gets measured through studies that compare vaccinated and unvaccinated people. Researchers look at how many people in each group get sick with flu. They express this as a percentage showing how much the vaccine reduces illness risk. The CDC uses these studies to tell people how well flu vaccines work each year.
Why do flu vaccines vary in effectiveness each year?
Flu vaccines work differently each year because flu viruses change. The main factor is how well vaccine strains match the viruses spreading in communities. Flu viruses mutate often, which can make vaccines less effective. When mutations change the virus too much from vaccine strains, protection decreases. Scientists monitor these changes and adjust vaccines when possible.
Can flu vaccines cause the flu?
No, flu vaccines cannot cause flu illness. Vaccines use either killed viruses or no virus at all. This makes it impossible to get flu from the vaccine. Some people might feel mild symptoms like fever or tiredness after vaccination. These are normal signs that the body is building protection, not flu illness.
What are the common side effects of flu vaccines?
Common flu vaccine side effects are usually mild and go away on their own. These include soreness at the injection site, low fever, and muscle aches. Serious side effects are rare. People with allergies or health conditions should talk to their doctors to make sure the vaccine is safe for them.
How long does protection from the flu vaccine last?
Protection from flu vaccines starts about two weeks after vaccination and usually lasts through flu season. Because flu viruses change and evolve, people need annual vaccination for best protection. Each year's vaccine targets the strains most likely to spread, giving the best possible protection for that season.
.png)



.png)
.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)
.png)

.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)

.png)
.png)
.png)

.png)

.png)


.png)







